HUNGER –
Hormonal Influences
The insulin response that happens after we start eating appears to be one factor in hunger. Insulin and glucagon are hormones that the pancreas secretes to control the whole body’s fat, protein, and carbohydrate levels, including glucose (blood sugar). For example, insulin decreases the glucose level in the bloodstream, whereas glucagon increases the level. Insulin, normally released in greater quantities after the beginning of eating, causes a feeling of hunger.
Because of the drop in the amount of blood sugar. Carbohydrates, particularly those that are simple or highly refined (such as table sugar, fruit drinks, white flour, and white bread or pasta), cause the level of insulin to spike even more than other foods, because these foods release so much glucose at one time. High blood sugar results in the release of more insulin, resulting in low blood sugar, increased appetite, and a tendency to overeat. That is the fundamental principle behind many of the diets that encourage low intake of carbohydrates. The proponents of these diets argue that they can control the insulin reaction and prevent it if people control the carbohydrates.
Later on, starvation cravings. A hormone called leptin has been identified in recent years as one of the factors that appears to regulate appetite. Leptin signals to the hypothalamus when released into the bloodstream that the body has had enough food, reduces appetite and increases the feeling of being full or satisfied.
The Role of the Hypothalamus
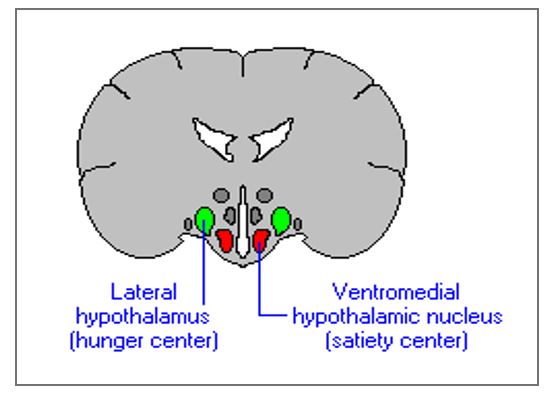
As a result of its influence on the pituitary, the role of the hypothalamus in controlling many kinds of motivational stimuli, including hunger, has been seen. But the hypothalamus itself has different areas that appear to control eating behavior, controlled by the levels of glucose and insulin in the body.
In order to stop eating, the ventromedial hypothalamus (VMH) may be involved.
Response when the levels of glucose go up. In one study, rats whose VMH areas were damaged (located towards the bottom and center of the hypothalamus) would no longer stop eating; they ate and ate until they were quite overweight. Actually, they became rather picky, overeating only on food that appealed to them. In fact, if they were unappealing with all the food available to them, they did not become obese and in
In some cases, weight has even been lost. When insulin levels rise, another part of the hypothalamus, located on the side and called the lateral hypothalamus (LH), seems to influence the onset of eating. Damage to this region caused rats to stop eating to the point of hunger. They would eat only if, under those circumstances, they were force-fed and still lost weight. Both of these hypothalamus areas are involved in the production of a neuropeptide (small, protein-like) called orexin-A.
(Molecule used by neurons to interact) involved in appetite control
 Weight Set Point and Basal Metabolic Rate
Weight Set Point and Basal Metabolic Rate
The hypothalamus’s role in eating behavior is obviously complex. Some researchers believe that the hypothalamus affects the specific weight level the body is trying to achieve called the weight set point, to preserve. Hypothalamus injury raises or decreases the set point of weight rather dramatically, causing either drastic weight loss or weight gain. At the weight set point, metabolism, the speed at which the body burns available energy, and exercise also play a role. To have faster metabolisms, some individuals are no doubt genetically wired, and those individuals can eat large amounts of food without gaining weight. Others have slower metabolisms and may eat and still gain weight or have difficulty losing a normal or even less than-normal amount of food. The slowing of the metabolism and the increase in the weight set point that comes with it can be offset by regular, moderate exercise. When a person is resting, the rate at which the body burns energy is called the basal metabolic rate (BMR) and is directly tied to the set point.
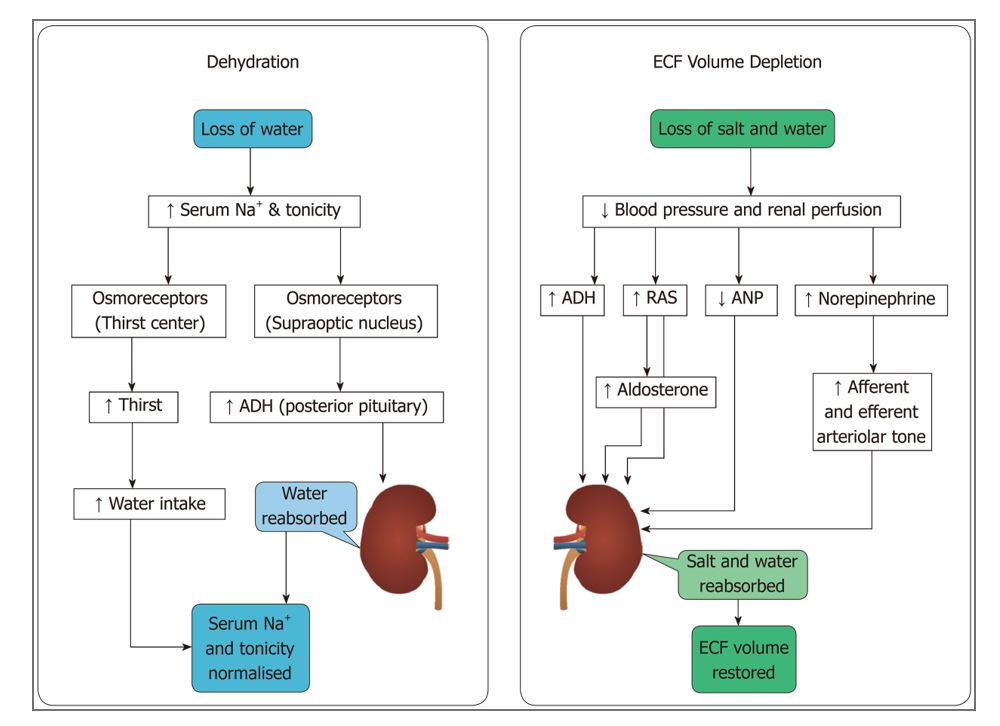
Thirst motivation is regulated by peripheral and central nervous system systems, like that of hunger. In part, thirst regulation includes a chemical (angiotensin) produced by the kidneys, a hormone (antidiuretic hormone (ADH), also referred to as vasopressin) produced by the pituitary gland, both the intra- and extra-cellular water content of the cells in the body.
Structures of the central nervous system, such as the subfornical organ and the LH (lateral hypothalamic nucleus), also help control thirst. Damage to the LH causes the animal to become adipsic and to become aphagic (failure to drink) (fail to eat). The hypothesis of double depletion contends that thirst is generated both outside and within cells by depletion of fluid.
Intracellular dehydration refers to water loss from inside cells and is usually caused by an increase in osmolality of the blood, which osmoses water from cells and causes them to shrink.
Extracellular dehydration, on the other hand, refers to a reduction in the total volume of blood, as is the case during bleeding. Whereas drinking water alone can correct intracellular dehydration, extracellular dehydration requires both water and salt consumption in order to regenerate the blood to its correct osmolality. Extracellular dehydration therefore causes not only thirst, but also salt appetite. Changes in blood osmolality correlate well with human subjective feelings of thirst, and the most important homeostatic signal for drinking in daily life is probably increased blood osmolality. When blood osmolality and volume defense are put into conflict, such as when blood volume and osmolality increase simultaneously, the body prioritizes osmolality defense, suggesting that under most circumstances, blood hypertonicity is the most immediate threat to survival.
SLEEP
Role of Hypothalamus
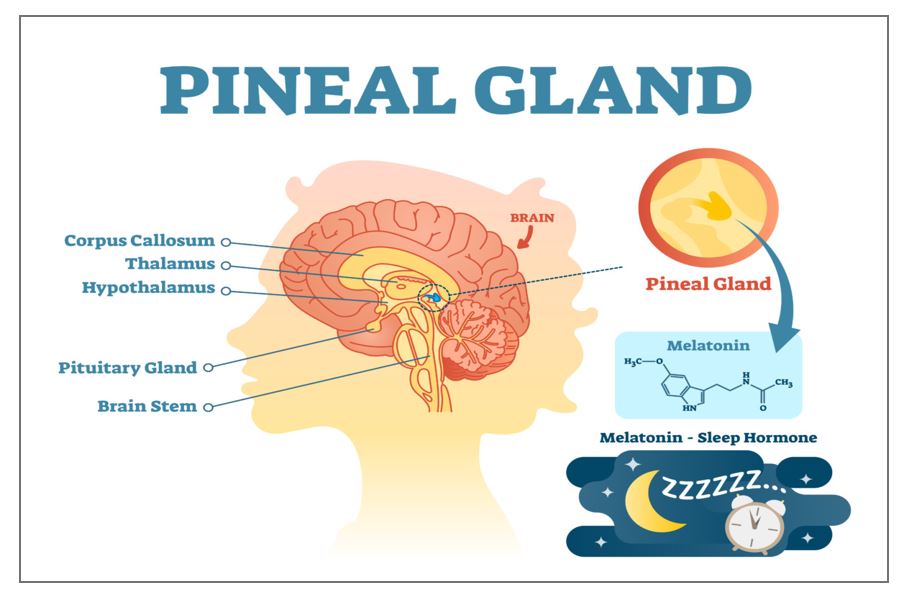
The release of melatonin is influenced by a structure deep within the tiny hypothalamus in an area called the suprachiasmatic (SOO-prah-ki-AS-ma-tik) nucleus, the internal clock that tells people when to wake up and when to fall asleep. The nucleus of the suprachiasmatic, or SCN, is sensitive to light changes. The SCN tells the pineal gland (located in the brain’s base) to secrete melatonin as daylight fades. A person will feel sleepy as melatonin accumulates. The SCN tells the pineal gland to stop secreting melatonin as the light coming into the eyes increases (as it does in the morning), enabling the body to awaken. For such a small part of the brain, that is a lot of control.
The adaptive hypothesis
Sleep theory suggests that sleep patterns have been changed by animals and humans to avoid predators by sleeping when predators are most active.
Restorative philosophy
Sleep theory suggests that sleep is necessary for the physical health of the
Body and serves to replenish chemicals and to repair damage to cells.
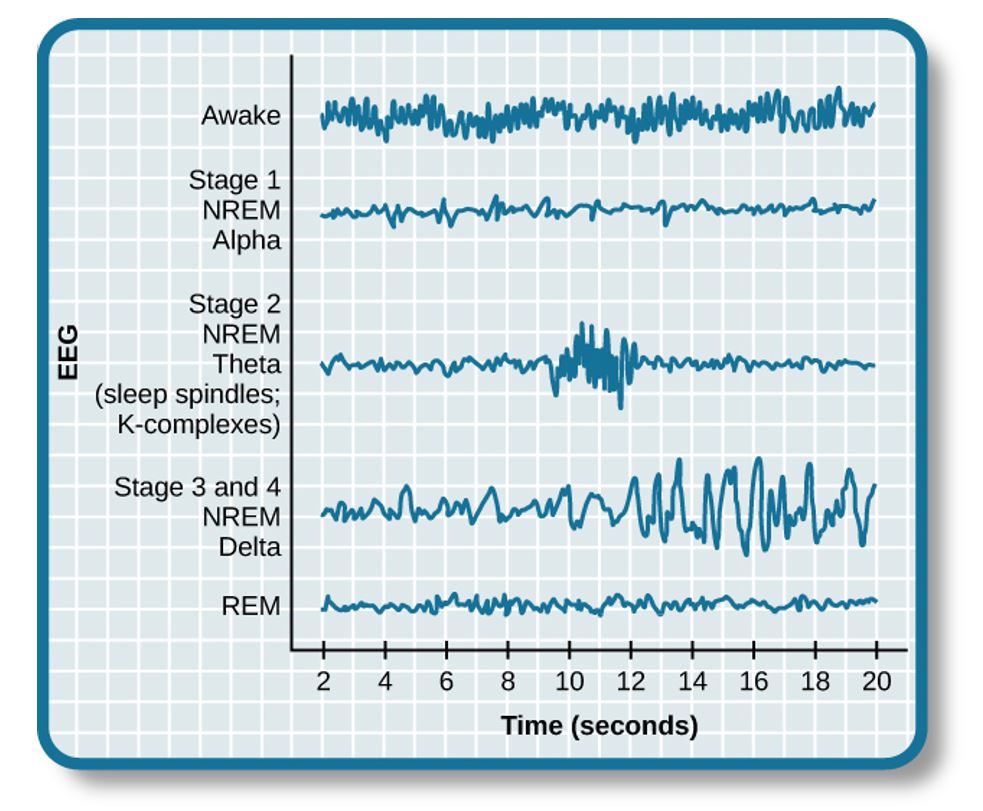
N1: Light Sleep As activity of the theta wave increases and activity of the alpha wave fades, People are said to enter stage N1 sleep, or light sleep, away from home. In this stage of sleep, several rather interesting things can happen. At this point, if individuals are awakened, they will probably not believe they were actually asleep. They may also experience hypnogogic images or hallucinations called vivid visual events. The Hypnic Jerk is a much more common occurrence. Did you ever drift off to sleep when your knees, legs, or your whole body gives you a big “jerk” sometimes? Although experts have no solid proof of why this occurs, many believe that it has something to do with the possibility that our ancestors slept in trees: The relaxation of the muscles as one drifts into sleep causes a “falling” sensation, at which point the body jerks awake to prevent the “fall” from the hypothetical tree.
N2: Sleep Spindles The body temperature starts to drop as individuals drift back into sleep. The heart rate slows down, the breathing becomes shallower and more irregular, and the EEG shows the first signs of sleeping spindles, brief activity bursts that last only a second or two. At this stage, Theta waves also predominate, so if people are awakened during this stage, they will be conscious that they have been asleep.
N3: Delta Waves The slowest and largest waves roll in in the third stage of sleep. During this stage, these waves rise from about 20 percent to more than 50 percent of total brain activity. The individual is now in the deepest sleep stage, often referred to as slow-wave sleep (SWS) or just deep sleep.
It is during this stage that growth hormones are released from the pituitary gland (often abbreviated as GH) and reach their peak. The body is at its lowest functioning level. Eventually, the delta waves for this stage of sleep become the primary brain function.
It is very difficult for people in a deep sleep to wake up. If something wakes them, they can initially be very confused and disoriented. In this kind of disoriented state, it is not uncommon for individuals to wake up only to hear the crack of thunder and recognize that a storm has come up. When children are in this state, it is even harder to wake up than adults. The time when body growth occurs is deep sleep. This may explain why children need to sleep more in periods of rapid growth and also helps to explain why children who experience disturbed sleep (as is the case in domestic violence situations) suffer growth delays.
R: Rapid Eye Movement The sleeping person will go back up through N2 after spending some time in N3 and then into a stage in which the body temperature rises to near-waking levels, the eyes move rapidly under the eyelids, the heart beats much faster, and brain waves resemble beta waves, the type of brain activity that usually signals wakefulness. In the stage known as rapid eye movement sleep (R) and sometimes referred to as paradoxical sleep, the person is still asleep.